In August of 2023, the League’s Board of Trustees voted to end the Health Benefits Trust (HBT) contract with its provider, MedCost, and transition to the League’s new provider partners, Aetna and Vimly Benefits Solution, effective July 1, 2024.
The League fully understands the uncertainty and questions that stem from such an important change. The decision to switch providers was not made lightly. This transition will allow League staff to have more involvement in eligibility and provide the ability to help members more directly, bringing a higher level of customer service facilitated by the League, to members.
“Taking billing, eligibility, and customer service in-house doesn’t only provide cost savings to our membership in future years; it’s an investment in fostering direct relationships, enhancing accountability, and driving positive change from within. We are excited about the future of this program and what we will be able to do for our membership with these changes,” says Youssou Fall, NCLM Director of Strategic Operations.
So, what does this mean for HBT members?
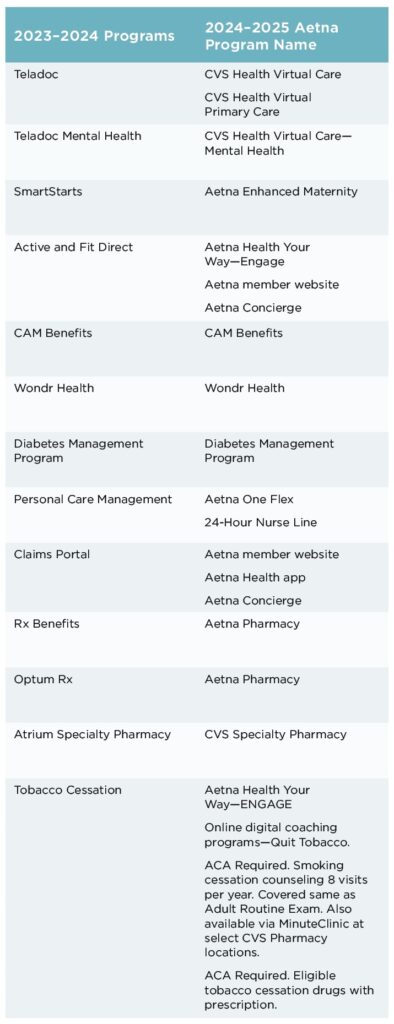
To modernize plan options with this transition, some benefits will be altered to have a more positive impact on members’ overall experiences. Members will still receive similar great plan options. One important change is the way these plan benefits are administered to members. For example, existing members are familiar with MedCost’s provider Teladoc as a virtual, on-demand care service. Aetna offers CVS Virtual Care and CVS Virtual Primary Care as their virtual, on-demand care provider. View the full list of new program names in the chart.
 Members can expect the same health care they are accustomed to under their current HBT plan offered by the League, including medical, dental, vision, pharmacy, life, and short-term disability benefits. Aetna’s expansive provider network will be able to offer members even more access in the 2024–2025 plan. Their provider network is a 99.6% match to providers previously offered through MedCost. The few primary care physicians not currently in Aetna’s provider network will be “grandfathered” in as in-network providers for current pool members. The bottom line is members will not have to change their primary care physician. With this greater network of new providers, members can get access to care that is conveniently located close to them, no matter where they are in North Carolina.
Members can expect the same health care they are accustomed to under their current HBT plan offered by the League, including medical, dental, vision, pharmacy, life, and short-term disability benefits. Aetna’s expansive provider network will be able to offer members even more access in the 2024–2025 plan. Their provider network is a 99.6% match to providers previously offered through MedCost. The few primary care physicians not currently in Aetna’s provider network will be “grandfathered” in as in-network providers for current pool members. The bottom line is members will not have to change their primary care physician. With this greater network of new providers, members can get access to care that is conveniently located close to them, no matter where they are in North Carolina.
Vimly Benefit Solutions, and its software platform named SIMON, will be the billing and eligibility vendor for all HBT plans. The SIMON software allows the League to bring eligibility in-house. This means that the League will use the SIMON platform to make any enrollment changes, such as new hires, terminations, and qualifying event changes on behalf of members.
Over 10 years ago, the League previously handled billing and eligibility in-house very successfully and efficiently.
CUSTOMER SERVICE
The League has a robust and expert staff that provides assistance in whatever capacity is needed from HBT members. League HBT Consultants knows that each member is unique and has a different set of healthcare needs from the next. League staff works to curate and implement the best plan for each of its members by working closely and diligently with municipal employers across North Carolina.
HBT Consultants have expert knowledge on how to make the most of each member’s plan. They can provide in-depth, specific knowledge on each program that is available to members and the best practices to utilize each service, all one phone call away.
“The customer service is just top-notch,” says Casey Warner, Town of Indian Trails Human Resources Director. “I always get an answer within a day, sometimes within 30 seconds.”
The Town of Indian Trails has been a member of the League’s Workers’ Compensation and Property and Liability Insurance pools for many years before deciding to also join the Health Benefits Trust. Because of the great past experiences Warner had with the League’s risk management staff, she trusted the League to provide health coverage to the Town of Indian Trails’ 53 employees.
 To get to know the needs and expectations of all HBT members, the League not only utilizes HBT Consultants but also League Business Services Consultants who are all licensed insurance producers. Consultants meet face-to-face with HBT members in their municipalities to assist them with any questions and provide risk management programming and knowledge of all the League’s programs and services.
To get to know the needs and expectations of all HBT members, the League not only utilizes HBT Consultants but also League Business Services Consultants who are all licensed insurance producers. Consultants meet face-to-face with HBT members in their municipalities to assist them with any questions and provide risk management programming and knowledge of all the League’s programs and services.
“We have [League consultants] come out every year and do open enrollment presentations, they handle all of that and it makes it very easy … and it’s always well-received,” says Warner. “If they don’t know an answer to a question, they’re going to find out, they don’t leave you hanging.”
Further, the SIMON platform fits varied plan needs and allows the League’s consultants to directly assist members with enrollment changes with a quick turnaround. If a member needs to add a new employee to its plan or terminate coverage, they can contact the League directly with this change. Members will also be able to log into the SIMON platform and make the change themselves. Either method allows the League to have access to this eligibility information and the ability to assist members when questions arise.
In February, the League’s HBT staff began hosting an ongoing webinar series that will showcase the strategic shift to Aetna and Vimly and demonstrate the transformative advantages this transition will bring. Some webinars include Aetna and Vimly representatives. This is a fantastic opportunity to meet the new HBT partners and understand the compelling reasons behind this exciting transition, ensuring that members are well-informed and confident in the positive changes ahead.
A recording of each webinar is available on the League’s website.
Additionally, the annual Risk Management Services (RMS) Spring Tour connects members with League staff throughout the state to discuss renewal offers for each insurance pool. This year, there will be a specific focus on HBT’s transition to Aetna. This is a great opportunity to ask League insurance experts any questions or address any concerns this transition brings.
For nearly 40 years, the League’s Health Benefits Trust has prioritized member needs and personalized customer service—that will never change. This transition will only strengthen those priorities and allow the League to provide enhanced service to all HBT members.














